Multiple sclerosis: what are the symptoms and available treatments?
Publication date: 01-08-2023
Updated on: 01-08-2023
Topic: Neurology
Estimated reading time: 1 min
Article Author
Clelia Andolina
Medical Editor
Massimo Filippi
Editor and Translator
Viktoryia LuhakovaMultiple sclerosis (MS) is an inflammatory, demyelinating, and neurodegenerative disease of the central nervous system, consisting of the brain and spinal cord, which manifests itself with a variety of symptoms at an early age as well as later in life. It is a chronic condition, from which there is no cure, but on which effective treatments have been developed that can decrease the frequency and severity of attacks, slowing their progression.
What is it, when does it occur, with what symptoms, and what treatments are available to date? We asked Prof. Massimo Filippi, director of the Neurology Unit, Neurophysiology Service and Neurorehabilitation Unit at Ospedale San Raffaele.
What is multiple sclerosis?
MS is caused by an abnormal functioning of the immune system, which, instead of activating toward external agents, attacks myelin, the substance that coats and protects nerve fibers and helps ensure efficient transmission of nerve stimulus throughout the body.
As a result of the attack by the immune system, tissue damage is created, which may be followed by the appearance of various symptoms, depending on the site where the episode occurred. The inflammatory component can be “reabsorbed” as well as remyelination and compensation processes develop, but scars, so-called plaques, still remain there.
At what age does it occur?
Typically, the disease first occurs in youth, between the ages of 20 and 40, but not infrequently it can have a late onset, after the age of 50. In addition, in about 5 percent of cases the disease may occur during the pediatric age. Women are affected in almost three times the number of men.
Symptoms
Symptoms depend on the site where the lesions develop, which is why they are extremely variable. The most common ones are:
- visual disturbances;
- alterations in strength and/or sensitivity;
- fatigue.
The patient, therefore, may experience such manifestations as:
- splitting of vision;
- sudden visual decline;
- alterations in eye movements;
- tingling;
- sensation of numbness in the limbs;
- lack of sensitivity;
- difficulty perceiving heat and cold;
- loss of muscle strength;
- tiredness;
- fatigue;
- disturbance of balance.
Genito-urinary problems, such as difficulty in retaining urine and/or feces and sexual disorders, are also common.
How does the diagnosis occur?
The diagnosis of MS is made by the neurologist after a careful evaluation, which cannot be separated from a thorough history collection, that is, a thorough interview with the patient, with the aim of learning about the patient's symptoms and medical history. Therefore, a complete neurological examination is performed.
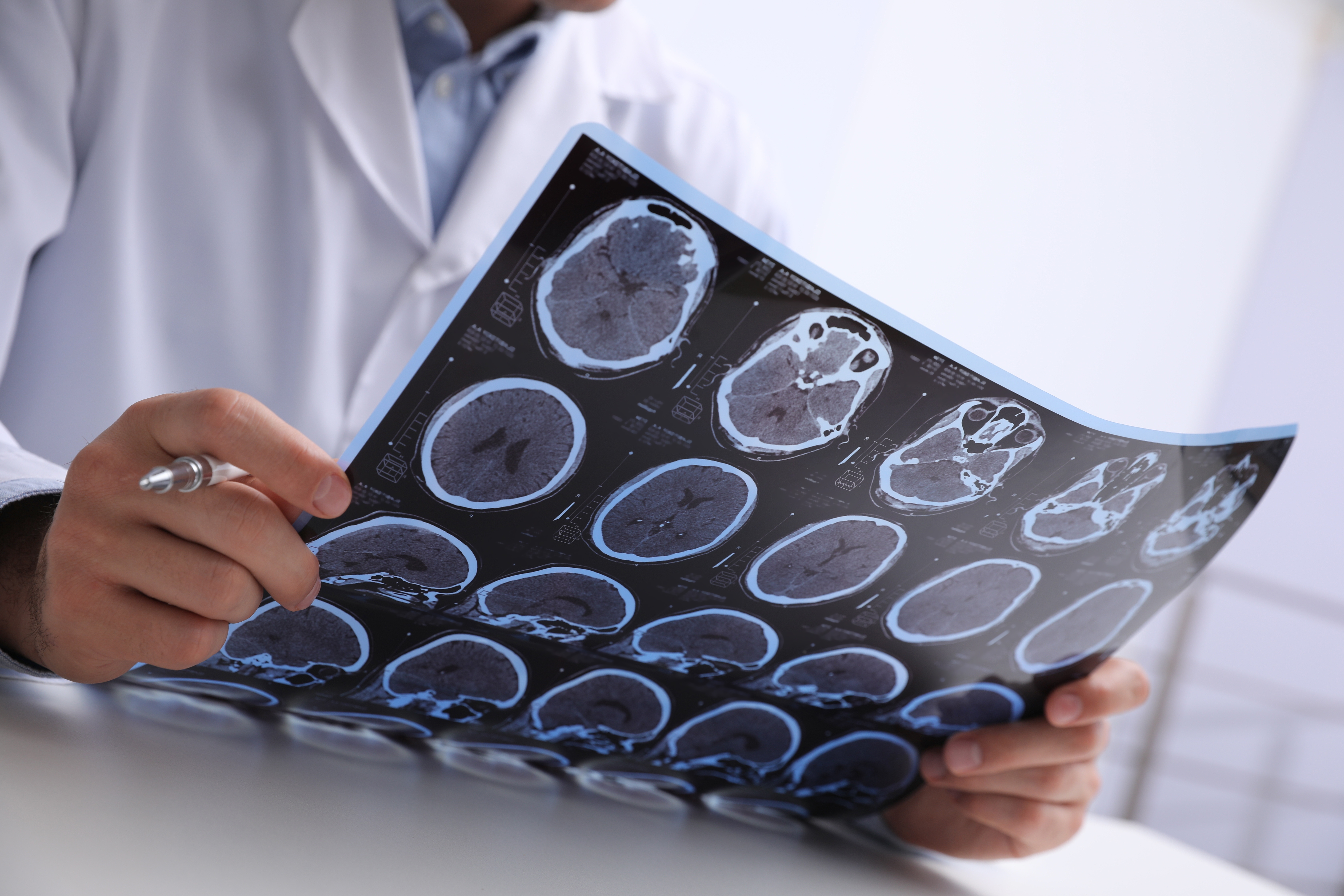
From the point of view of instrumental examinations, the pivotal assessment is MRI of the brain and spinal cord, which can identify even subclinical lesions. To complement this, other examinations are used:
- evoked potentials, which measure the speed of conduction of nerve stimuli along nerve fibers;
- an examination of the cerebrospinal fluid, which allows for identification of possible markers of immunopathology within the central nervous system.
Possible causes
MS is a multifactorial disease, that is, due to the interaction of genetic and environmental factors. To date, more than 300 genes have been identified that are associated with an increased predisposition to develop the disease. As for environmental factors, only some of the concomitant causes that can trigger the autoimmune mechanism underlying the disease are known, such as:
- viral infections;
- overweight and obesity especially in adolescence;
- vitamin D deficiency;
- cigarette smoking;
- living far from the equator.
Existing forms of the disease
Based on the clinical course and progression, different forms of MS can be distinguished. The most common form is the relapsing-remitting form, which alternates between phases of acute inflammation and demyelination, so-called relapses, in which there is the appearance of new disorders or worsening of existing symptoms, and phases of remission and recovery, in which some manifestations may disappear completely. Over the years, this form can evolve to secondarily progressive MS, which is characterized by a progressive and worsening accumulation of disability over time.
Then there are other forms that present with a progressive course from onset and are termed primarily progressive. There are predictive factors that help guide prognosis, but the best approach is careful monitoring that looks at the specific aspects of the disease in the individual case.
Available treatments
MS is a chronic, severe and progressive disease from which there is no cure. However, today we have effective treatments available that can decrease the frequency and severity of attacks, slowing the progression of the condition.
In fact, in the last 20 years, we have seen a radical change in the treatment scenario of MS, and we currently have several drugs available to control the evolution of the disease, and we will have more in the future, as research is very active in this area. The available molecules essentially belong to 2 classes: immunosuppressants and immunomodulators, which act, through different mechanisms of action, by keeping the immune system in check and thus hindering the central nervous system damage caused by the disease.
The choice of treatment involves an approach designed to ensure the most personalized treatment possible, taking into account the individual patient's disease characteristics as well as his or her needs and lifestyle habits. To date, we have numerous data indicating that it is critical to start effective treatment early to reduce disease activity and significantly prevent the accumulation of disability.